Registered nurse Kevin Hoover puts on protective gear as he prepares to check on a COVID-19 patient May 20 at the rural 24-bed Kearny County Hospital in Lakin, Kansas. The county has seen a spike in cases due to clusters in nearby meatpacking plants. (AP Photo/Charlie Riedel)
A little over four years ago, the city of Streator, Illinois, lost its only inpatient health care facility.
St. Mary's Hospital, a Catholic provider, closed in January 2016 after serving the city of roughly 13,800 inhabitants and its surrounding communities since 1887, according to the Herald and Review of Decatur, Illinois.
"It's tough for somebody that was born in this hospital and had their families here, maybe for 50 years," said Streator Mayor Jimmie Lansford. "And then all of a sudden, boom, we don't have it."
The hospital building has reopened under new Catholic ownership as OSF Center for Health-Streator, and the building was renovated. The facility now offers emergency room and primary care services.
But it no longer offers inpatient care, according to Don Damron, OSF HealthCare's vice president of ambulatory services. The closest two inpatient facilities are now roughly 15 and 25 miles away.
In the midst of the global COVID-19 pandemic, Streator, like many rural communities across the country, lacks inpatient medical care, including equipment like ventilators. Patients with severe COVID-19 often need a ventilator to help them breathe and keep them alive.
For Streator's residents, Damron said, the closest ventilator is 15 miles away.
An ongoing trend
St. Mary's is just one of dozens of rural hospitals that have succumbed to financial strain in recent years. Since 2015, 85 hospitals in rural areas have closed, according to data collected by researchers at the University of North Carolina.
The trend of hospital closures has only been accelerating during the pandemic — just as COVID-19 infection rates have begun to spike in rural areas. With 15 closures as of October, 2020 is on track to eclipse the previous record for closures set in 2019, when 18 rural hospitals shut their doors, according to University of North Carolina researchers.

An aerial view of OSF Center for Health-Streator in Streator, Illinois. The nearest inpatient facility for most residents of Streator is OSF's hospital in Ottawa, Illinois — roughly 15 miles away. (Courtesy of OSF)
Prior to the pandemic, rural hospitals were already in deep trouble, said Alan Morgan, CEO of the National Rural Health Association. Nearly 75% of U.S. critical access hospitals — certain rural hospitals with fewer than 25 general-use beds located far from other facilities — were operating at a loss going into the pandemic, according to an analysis by a group of nonprofit newsrooms.
As many as 25% of rural hospitals — about 350 facilities — were at risk of closing due to their financial situations, according to a study by the consulting firm Guidehouse, including over half of the rural hospitals in Tennessee, Alabama, Oklahoma and Arkansas.
"We were looking at a horrific situation for the nation's rural hospitals," Morgan said.
Catholic role in rural care
There's little reliable data on how many recently shuttered rural hospitals have been Catholic. But Catholic hospitals play a major role in providing health care in rural areas.
According to the patient advocacy group MergerWatch, roughly 10% of all "sole community hospitals" are Catholic hospitals. In some states with large rural populations — such as Iowa, Kansas, Wisconsin and Alaska — over 40% of acute care beds are in hospitals run by or affiliated with Catholic organizations, according to MergerWatch.
There are more than 670 facilities listed in the hospital database for the Catholic Health Association, roughly 200 of which are in zip codes designated as rural by the Federal Office of Rural Health Policy. Of these rural Catholic hospitals, 36 are on the list of "sole community hospitals" created by MergerWatch in 2016.
The map below shows the Catholic Health Association member hospitals that are located in rural zip codes. Orange dots represent those designated as sole community providers by MergerWatch.
"We have a strong and long history of commitment towards rural populations," said Nathaniel Hibner, director of ethics for the Catholic Health Association. "This comes obviously from the Catholic commitment to meeting the needs of everyone — the preferential option for the poor and vulnerable."
Some advocates — such as the American Civil Liberties Union — have said some Catholic ethical guidelines may prohibit crucial, even lifesaving care based on religious principles that not every patient shares.
The U.S. Conference of Catholic Bishops' Ethical and Religious Directives for Catholic Health Care Services state, for instance, that abortion is never permitted, even in the case of rape or medical emergency.
The guidelines also prohibit Catholic providers from promoting or condoning contraception or from directly sterilizing anyone.
Some transgender people also report experiencing discrimination and even being denied health care in Catholic hospitals, which are the only option for many people living in rural areas.
Oliver Knight, a trans man in the small city of Eureka, California, wrote in a blog post on the American Civil Liberties Union website that his hysterectomy — which he'd scheduled as part of his transition process — was canceled after he was already hooked up to an IV and ready for the procedure, all because of the hospital's Catholic ethics.
"I felt humiliated and queasy as I sat on the curb waiting for my roommate to pick me up," Knight wrote. "It seems the hospital does not understand how it feels to be treated inhumanely just because your body parts do not match your soul."
Advertisement
Knight is one of several trans people in recent years to sue Catholic hospitals for denying health care.
The Catholic presence in rural health care had grown before the pandemic. Between 2001 and 2016 the percentage of all hospitals run by Catholic organizations increased, according to a 2016 report by MergerWatch. While the overall number of hospitals fell during that time period by about 6%, the number of Catholic hospitals grew by 22%.
A 'lifeline' that hasn't been enough
As the pandemic began to hit the United States, hospitals began to limit or cancel non-emergency procedures to prepare for a wave of COVID-19 patients and protect patients and staff members from contracting the virus. The pandemic has had a severe impact on the financial health of institutions that relied on non-emergency procedures to improve their bottom lines.
Some administrators thought funding for treating COVID-19 patients might compensate for the lack of elective procedures, said Bob Ritz, CEO of MercyOne, a Catholic hospital network with facilities across Iowa, including many in rural communities.
In fact, nearly the opposite was true. Ritz said his network lost roughly $175 million in revenue from canceled procedures. Federal aid, he said, only made up for about half of that shortfall.
"I don't believe that will ever be recovered," he said.
Although the Coronavirus Aid, Relief, and Economic Security (CARES) Act provided $175 billion in relief for hospitals dealing with COVID-19, only around $11 billion of that was specifically allocated to hospitals serving rural populations, according to the U.S. Department of Health and Human Services.
While it was a "lifeline," to many rural providers, this federal funding wasn't enough to stem the tide of rural hospital closures, said Dr. Adrian Diaz of the University of Michigan Institute for Healthcare Policy and Innovation.
The financial impact from COVID-19 has only exacerbated hits to rural hospitals' bottom lines, caused by other factors.
How did rural hospitals wind up in such dire financial straits in the first place? According to researchers at the Kaiser Family Foundation, people who live in rural areas are generally older and tend to make less money on average than those in urban areas.
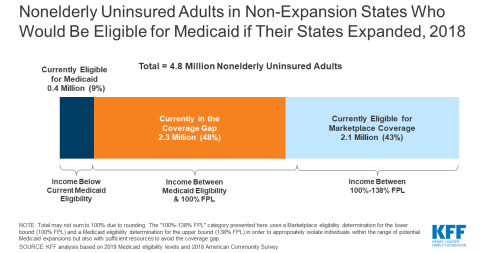
The states with the highest rates of rural hospital closures are often those that haven't taken the option offered by the Affordable Care Act to expand Medicaid to people whose incomes are just above the federal poverty line, Diaz said.
These states are mostly in the South and tend to have higher percentages of Black residents than do states that have expanded Medicaid, according to the Kaiser Family Foundation. Black Americans, along with Latino and Indigenous people, are more likely to be uninsured than their white counterparts, according to the foundation.
States that haven't expanded Medicaid leave out people who are still well below the federal poverty line and can't afford other insurance options, according to the Kaiser Family Foundation. This hurts patients who can't afford to pay out of pocket for doctor's visits, and it can also hurt hospitals. Treating uninsured patients can place a major strain on a hospital's finances, Diaz said.
"Many of these hospitals are treating patients that might otherwise be eligible for Medicaid," Diaz said. "Most ... [or] all that care ends up being uncompensated care."
Rural hospitals in states that hadn't expanded Medicaid saw an average operating margin of -0.3%, compared with positive 0.8% in states with Medicaid expansion, according to the Chartis Center for Rural Health.
A crisis intensifies
Hospital closures have placed rural communities in a precarious position as COVID-19 infections begin to spike outside major cities.
While COVID-19 initially hit urban areas harder than rural ones due to population density, Morgan said, rural areas are starting to see a spike in cases, matching or exceeding urban areas in recent weeks, according to an analysis by the Daily Yonder.
Many of the counties with the highest infection rates are now in rural areas, according to data from Johns Hopkins University.
When people from urban areas think of rural America, they typically think of a rancher in Nebraska, completely removed from other people, Morgan said. But that's not usually the case — most rural Americans live in "three-stoplight" towns where people go to all the same stores together and viruses can spread easily.
"For a lot of rural communities ... you're talking elderly populations, with multiple chronic health conditions — a disproportionate share of the population are those most at risk for COVID," Morgan said. "Once COVID is brought into these communities, it's just been like throwing a match on a tinderbox."

Dr. Monica Baskin, professor at the University of Alabama at Birmingham School of Medicine (UAB)
COVID-19 death rates were higher in rural counties with larger shares of Black and Latino residents, according to a recent study. People of color make up about 20% of the rural population.
Historical and ongoing discrimination in housing, employment and the health care industry itself has created a situation where people of color in rural areas are less likely to have ready access to health care, said Dr. Monica Baskin, a professor at the University of Alabama at Birmingham School of Medicine. Due to these social and environmental factors, Black and Latino rural residents also have higher rates of chronic conditions putting them at risk of complications from COVID-19, she said.
Hospital closures can have a devastating impact on rural community health even outside of a pandemic. One study found, for instance, that mortality rates in rural communities rose by nearly 6% when local hospitals closed.
When someone has an emergency — such as a heart attack — minutes and seconds can be the difference between life and death, Baskin said.
"As more and more of the rural facilities are closing down, it is very concerning that someone may literally have to go to the next county or two counties over in order to get that care when they need it," she said.
In rural Perry County, Alabama, many people live far from the nearest emergency room after a critical access hospital closed 15 to 20 years ago, said Keshee Dozier-Smith, CEO of the Rural Health Medical Program Inc., a network of community health care facilities in Alabama. There are only two ambulances for the entire county.
"If there are 10 calls that come in, they have to take the most urgent," Dozier-Smith said. "That patient that was not prioritized is impacted. And that's unfortunate, but that service is doing the best that it can."
Jack Dzuris, executive director of the Chamber of Commerce in Streator, Illinois (OSF Healthcare)
Hospital closures can also make it more difficult to get to routine appointments, Baskin said. If the nearest hospital is hours away, people might need to take a day off work to see their doctor for a routine checkup, which might not be financially possible. They might also have trouble getting transportation, and if someone else has to drive with them, it can mean two days' worth of lost wages.
In Streator, the nearest inpatient care is 15 miles away, Damron said.
"It's not ideal, it's not the same as driving seven minutes like I used to," said Jack Dzuris, executive director of Streator's Chamber of Commerce.
Streator residents with head trauma are typically taken to Peoria — roughly 60 miles away. For burn injuries, they're often transported as far as Rockford — a Chicago suburb nearly 100 miles from Streator — said Mayor Jimmie Lansford, who worked at St. Mary's for more than 30 years until 1996.
Hospital closures can also have a major impact on the local economy. For instance, when St. Mary's in Streator closed, roughly 100 of the 290 people it employed weren't hired back by OSF, according to the Herald and Review.
Some of those who were rehired no longer have the same hours or benefits, Dzuris said.
Baskin noted that many of these layoffs hit nonmedical employees such as administrative staff, clerks and gift shop workers, creating ripple effects especially in smaller communities where hospitals are often major employers. Dzuris, who supported St. Mary's closure, chalked the layoffs up to the nature of the health care industry.
"How do you make money?" he said. "One of those ways is by reducing staff. ... I'm not saying it's right, but if you watch mergers that's what usually happens."

People walk outside the renovated facility of OSF Center for Health-Streator in Streator, Illinois. (Courtesy of OSF)
Saving rural health care
In response to the crisis in rural health care and the COVID-19 pandemic, researchers and advocates have pushed federal and state governments to step in while also reimagining the future of health care in rural areas.
Diaz said one way governments could help rural hospitals survive in the short term is by relaxing the definition of "critical access hospitals" — the very small, remote hospitals that are reimbursed at slightly higher rates by Medicare.
States could also choose to expand Medicaid to include people with incomes up to 138% of the federal poverty limit, to allow more people to get health insurance and make sure that rural hospitals are reimbursed for every patient they care for, Diaz said.
Medicaid expansion has also been a major policy goal for the Catholic Health Association, Hibner said.
In some rural areas with long drives to the nearest hospital, community health centers have filled in some of the gaps in everyday health care.
Dozier-Smith said her organization's community health care centers work with hospitals in larger urban centers to provide health care that's affordable for everyone, including people who don't have insurance. They offer sliding-scale fees and forge agreements with other providers to care for community members at reduced prices.
Lately, they've also been offering COVID-19 testing, she said, including a mobile unit that goes out to the most remote parts of their community.

Keshee Dozier-Smith, CEO of the Rural Health Medical Program Inc. (RHMPI)
Dozier-Smith herself grew up in Perry County, Alabama, and remembers going to a community health center run by the Rural Health Medical Program when she was a kid. Now, as an adult, she emphasized that community health centers aren't just for people who are experiencing poverty, and they hire licensed professionals, not volunteers or students. The basic principle is equity.
"We take care of people with Blue Cross Blue Shield the same way we take care of people that do not have money to actually pay for services, because our goal is to make sure that we're there to take care of the entire community," Dozier-Smith said. "We just definitely have a heart for those that are unable to pay."
During the pandemic, Dozier-Smith said, the Rural Health Medical Program has been working on expanding telehealth services — allowing people to meet with their doctors over the internet.
In response to the pandemic, the Centers for Medicare and Medicaid Services expanded the list of telehealth services federal programs will cover during COVID-19. Diaz said he thinks this could be part of a new wave in rural health care that could make it easier for people in very remote areas to do doctors' visits and allow rural providers to conference-call with more experienced doctors in urban areas on more complex cases.
As rural hospitals consolidate, some networks like OSF have physicians who live in urban areas but hold office hours in more rural branches, Lansford said. He said he knows it's hard to get doctors to move to places like Streator, and that telehealth and other innovations can be useful, but he sometimes longs for the "personal touch."
"I liked my doctor," Lansford said. "I liked to know who he was and that I could get ahold of him anytime I wanted to, and he would know my medical history — and know me personally."
Ultimately, Lansford said a little wistfully that he recognizes the economics behind rural hospital closures.
"You can say what you want, you can like it or you don't like it, but it's inevitable," he said. "I still think that small is beautiful."
[Madeleine Davison is an NCR Bertelsen intern. Her email address is mdavison@ncronline.org.]