A health care worker administers COVID-19 vaccines at a mass vaccination site in Ridgefield, Washington, Jan. 27. (CNS/Reuters/Alisha Jucevic)
Dr. Diana Cejas still gets nightmares about her stint on a ventilator, years after she survived cancer and a stroke.
The idea of going through that again as a COVID-19 patient terrified her.
So when she got her final dose of the COVID-19 vaccine Jan.14, Cejas said it felt like a weight had been lifted off her shoulders.
She documented the moment on Twitter, posting pictures with the caption "Disabled. Doctor. *Fully* vaccinated."
"Part of me just wants to run around and be like ... 'Give this person the vaccine!' " said Cejas, a pediatric neurologist who works at the University of North Carolina Chapel Hill. "We should be giving this on the street corner at this point. Because if it can keep someone else from getting that sick, I don't see why we can't be getting it to the people that need it the most."
But Cejas and many other experts and advocates warn that disabled people and communities of color in the U.S. are already being left out of the early vaccine rollout, even though the virus has disproportionately harmed them.
Dr. Akilah Jefferson Shah, an allergist and immunologist who is also an expert in health policy and bioethics, has "major concerns" about the vaccine rollout. "If things progress the same way that things progressed in other dimensions of this pandemic, then we are in major trouble."
Only about 8% of the population has had even one shot of the vaccine, and accurate data on vaccination by race or disability is scarce. The vaccine is also largely restricted to groups like health care workers, the elderly, and those deemed essential workers, such as teachers and grocery store workers.
But early signs indicate that affluent white communities are already getting the vaccine ahead of those hit hardest by the virus.
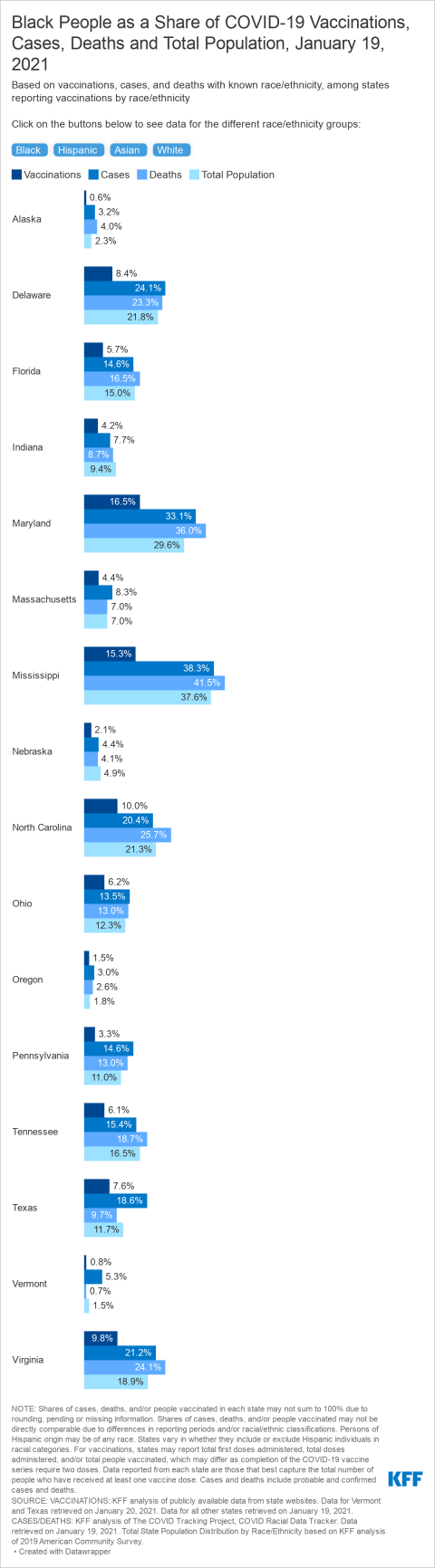
In Mississippi, Black people had only received 15% of the vaccines distributed, despite making up 42% of the state's COVID-19 deaths, according to a Jan. 21 report by the Kaiser Family Foundation. In Delaware, Black people had received only 8% of the vaccines despite accounting for nearly a quarter of the deaths. In fact, the report showed that Black people in all 17 states for which data was available were not getting the vaccine at rates proportionate to their infection rates.
"Together the data raise some early warning flags about potential racial disparities in access to and uptake of the vaccine," researchers said in the report.
In Chicago, a bot created by the South Side Weekly maps COVID-19 vaccination and death rates by zip code. The two maps, placed side by side, look like photographic negatives of one another. The Black and Latino neighborhoods with the highest death rates are not getting the vaccine as quickly as wealthy white ones.
Wealthier communities, with more clinics, grocery stores and hospitals, "are getting the vaccine more, but they have the lowest rates of COVID," Cejas said.
Disabled people, particularly those with conditions that make them more susceptible to the virus — such as cancer, organ transplants, HIV, diabetes, heart and lung diseases and developmental disabilities — have also raised concerns about the distribution process.
On Jan. 26, Gov. Gavin Newsome of California announced a new set of guidelines for vaccine distribution in the state that prioritizes age over health conditions. People under 50 who have disabilities or chronic illnesses that compromise their immune systems will be pushed to the back of the line, along with some essential workers, according to CalMatters. The state's vaccine working group simultaneously reduced the percentage of doses it had recommended to be earmarked for marginalized communities.
In response, younger disabled people and others in California, led by activist and editor Alice Wong, took to Twitter, using the hashtag #HighRiskCA to protest their exclusion from high-priority categories.
"I am 22, disabled, and immunocompromised," Stanford student Ariela Algaze wrote on Twitter. "Because of the pandemic, I no longer have access to regular medical care, and COVID-19 could kill me if I got it. Gavin Newsom just sent me to the back of the line to get vaccinated."
Some described living in extreme isolation for months, unable to leave home except for emergencies, or having to brave hospitals overflowing with COVID-19 patients to get lifesaving health care.
"The nice thing about being a heart surgery survivor on a lifetime regime of hardcore blood thinners at age 23 is that I might avoid my quarter-life crisis by dying while waiting in CA's new COVID vaccination line," activist and writer Kate Alexandria wrote on Twitter.
Elizabeth Schiltz, a board member at the National Catholic Partnership on Disability and a law professor at St. Thomas University in Minnesota, said she also worries that as the vaccine becomes more widely available, people who are unable to leave their homes may have difficulty accessing vaccination sites.
"They're talking now about having people come to big stadiums or line up, but what if you don't drive?" she said. "What if you don't have anyone to take you?"
To get the vaccine, people need reliable transportation and free time to get to their appointments, Cejas said.
Cejas said many people, especially in rural areas, don't live near major vaccine distribution centers, such as hospitals. Food deserts, more common in communities of color, may not even have a local grocery store or pharmacy. This can make it challenging to get to an appointment, she said. Many of her patients with disabilities find it difficult to make the trek to the hospital from rural parts of the state.
Furthermore, seeing the disparities in early vaccination rates may further erode trust in the medical system among communities of color and disabled people, Cejas said. Black people and other people of color, as well as disabled people, have suffered and continue to suffer systematic abuse and discrimination at the hands of the medical system, she said.
Scholars have documented centuries of abusive experimentation, health care segregation and coercive reproductive policies based in racism and ableism. Studies and personal narratives reveal ongoing medical discrimination that results in devastating outcomes such as higher maternal mortality rates for Black and Indigenous women and care rationing that devalues disabled lives.
Advertisement
Understandably, Cejas said, some people of color and disabled people are wary of the medical industry and anything associated with it — including the COVID-19 vaccine. Yet health care systems have done little to prove that they have changed and are now trustworthy, she said.
She worries that seeing the early signs of inequity in the vaccine rollout will only confirm marginalized communities' understanding that the medical system does not care about them.
"All that is saying is, 'See? We are right to not trust, we're right to not want this vaccine. This is not for us. The medical system wants nothing to do to help us,' " Cejas said.
This violated trust could make it more difficult to achieve the high vaccination rates needed to reach herd immunity and protect the U.S. population, surveys suggest.
Many bioethicists, including Catholics, argue that governments need to take into account the disproportionate impacts of the pandemic in distributing the vaccine.
Charles Camosy, associate professor of theological and social ethics at Fordham University, said Catholic social teaching urges care for marginalized members of society. He said this basic principle should guide distribution plans.
"Preference should be given to those who are most vulnerable to this virus: the elderly, the disabled, and those with comorbidities," he said in an email to NCR. "Beyond that, we should focus on racial minorities, essential workers, and others who have been traditionally disadvantaged in a more structural way."
The Vatican has also called for equitable distribution of the vaccine, particularly to those who are most vulnerable to the virus.
An Orange County firefighter in Irvine, California, holds his vaccination card after receiving the coronavirus vaccine Jan. 27. (CNS/Reuters/Lucy Nicholson)
"It is a matter of justice," Cardinal Peter Turkson, head of Pope Francis' COVID-19 task force, told Catholic News Service. "This is the time to show we are one human family."
Care workers who assist disabled people in their homes should be prioritized along with other health care workers, as they are disproportionately people of color themselves and often have multiple clients with compromised immune systems, said Adam Glickman, secretary-treasurer of the SEIU 775, a union representing long-term care workers in Washington and Montana.
"From a public health angle and a stopping the spread angle, vaccinating home care workers is important," Glickman said. "And then layer on top of that the equity lens of who are the people who are most vulnerable to the coronavirus and have fewer resources to be able to navigate the health care system."
Cejas said keeping disabled or high-risk people safe also means prioritizing people who are part of their informal care networks, such as family members.
Harold Braswell, a bioethicist at St. Louis University, said there is a "justice claim" for why disabled people and people of color should be prioritized in vaccine rollout plans.
"We should also consider the historical context and the social context that has led some groups to be disproportionately impacted, and realize that they've been done wrong, and that, therefore, there's a special obligation to be aware of their needs," Braswell said.
Studies suggest that Black, Latino, and Indigenous people have been dying of COVID-19 at much higher rates than white people due to histories of segregation and land theft — and ongoing structural racism in areas like employment, housing, and the medical industry.
Black people and other people of color are overrepresented as essential workers at high risk of being infected, according to the Economic Policy Institute. People of color have lost more jobs during the pandemic than whites, according to the Urban Institute, leaving them disproportionately uninsured and facing eviction, which can increase the likelihood of dying from COVID-19.
Disparities in health care access, racism in hospitals, and the stress of experiencing daily racism and economic oppression can also raise the risk of death, studies suggest.
"We as a society, government, et cetera, created these unjust conditions that have led to disproportionate impacts," Braswell said.
After adjusting for age, Pacific Islanders and Latinos were 2.5 times as likely to die of COVID-19 as white people in the United States. Black people were 2.3 times and Indigenous people 2.2 times as likely as whites to die of the virus, while Asian Americans died at a slightly lower rate than white people, according to a study by APM Research Labs that looked at data through Jan. 5, 2021.
At the time of the study, COVID-19 had claimed the lives of around 355,000 Americans, including 1 in every 595 Indigenous people in the U.S. and 1 in 735 Black people.
More than 80,000 additional people had died of COVID-19 in the U.S. as of Feb. 1, according to the Centers for Disease Control and Prevention.
While there is little data on COVID-19 death rates among disabled people in the U.S., and not all disabled people are inherently high-risk, some disabilities have been linked to increased likelihood of death from the virus.
Chronic illness, cancer, HIV, organ transplants, diabetes, and heart and lung conditions can all increase a person's risk of dying from COVID-19, according to the CDC.
Disabled or elderly people of color are also more likely to live in underfunded nursing homes and congregate care settings where they are more vulnerable to infection, Braswell said.
"Part of the process of reversing those social circumstances and repairing the wrong that's been done to these populations, both during and before the pandemic, is to prioritize them to the degree reasonable in vaccine distribution," Braswell said.
The first step in addressing inequities, Jefferson Shah said, is to collect accurate data. As of Jan. 19, only 17 states had released vaccine data that included race, according to the Kaiser Family Foundation. States need to get a lot more specific and include patients' race, age, occupation, ability status, and whether they live in an urban or rural setting, she said. Without it, policymakers won't know what's going on.
"There are some places that are collecting really good data, and a lot of places that are just simply not doing it," Jefferson Shah said. "And I don't think that's acceptable."
The Biden administration's new COVID-19 response plan has given Jefferson Shah and others some hope. It establishes a COVID-19 Health Equity Task Force and calls for data collection and increased focus on marginalized communities, including people of color and disabled people.
"That gives states a really good blueprint for what they need to be thinking about when they make their plans," Jefferson Shah said. "And of course, states have already made many plans. But those should be amended if they're not including looking at equity issues."
Cejas said in order to get the vaccine to people who do not have ready access to the usual distribution sites such as grocery stores, pharmacies and hospitals, health care providers need to meet people where they are.

Residents of William Reid Apartments in the Brooklyn borough of New York City rest for a few minutes after receiving the first dose of the COVID-19 vaccine Jan. 23. (CNS/Mary Altaffer, Pool via Reuters)
"When it's Girl Scout cookie time, you see those kids everywhere," Cejas said. "So why can't we just have something like that, where we have community-based rollout of vaccination programs, and we make it easy for people to get to."
A few state and local governments have created mobile vaccination units to bring vaccines directly to people's neighborhoods, particularly in rural areas. Some health networks are reserving a certain percentage of vaccine sign-ups for neighborhoods hit the hardest by the virus to counteract line-jumping. And local governments are enlisting community organizations, including churches, to help build trust and distribute the vaccines.
"Honestly, public health practitioners are going to have to get pretty creative," Cejas said. "And I know that we can, I just need to see it."
Ultimately, experts say getting everyone vaccinated is a matter of caring for the community. Francis has said Catholics should make the "moral choice" to take the vaccine when it's offered to protect those around them. Each person who gets vaccinated is helping to safeguard their loved ones and neighbors, Jefferson Shah said.
"[In] a public health crisis, we have to work as a collective public to get things under control," Jefferson Shah said. "And if we continue to work as individual units, we're not going to be able to get this thing under control."